|
Services |
Periodontology
What is periodontal disease?
The word “periodontitis” literally means “inflammation around the tooth”. Periodontal diseases are bacterial gum infections that destroy the attachment fibres and supporting bone that hold your teeth in your mouth. The toxins are penetrating the tissue and as soon as they entering the gum the body defense cells are trying to fight the foreign invading material and are forming an inflammation. This will then cause the gum to detach from the tooth thus causing a gap that is called a Pocket. Pockets in the range of 1-3mm may be normal. 4-5mm pockets usually need the attention of a hygienist and as the pockets progress, the consultation of a periodontist is required for evaluation of the severity of the disease with possible surgical intervention. Many people over the age of 35 develop periodontal diseases (80% of population). Periodontal diseases are painless until at their advanced stages. If left untreated, periodontal diseases can result in tissue and bone destruction and eventually tooth loss. In fact periodontal diseasses are the leading cause of adult tooth loss. The following are the most common symptoms of periodontal diseases: – Bleeding gum during brushing or flossing; – Persistent bad breath; – Red, swollen or tender gum; – Pus between the teeth and gums (leaving a bad taste); – Gum recess; – A change in the way your teeth fit together when you bite; – Loose or separating tooth. If you have any of the above symptoms, you should see a periodontist for a complete periodontal evaluation and proper treatment.
Periodontal treatment
Because gum disease is usually painless, however, you may not know you have it. Gum disease is caused by plaque, a sticky film of bacteria that constantly forms on the teeth. These bacteria create toxins that can damage the gums. In the early stage of gum disease, called gingivitis, the gums can become red, swollen and bleed easily. At this stage, the disease is still reversible and can usually be eliminated by daily brushing and flossing. In the more advanced stages of gum disease, called periodontitis, the gums and bone that support the teeth can become seriously damaged. The teeth can become loose, fall out or have to be removed by a dentist.
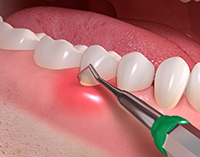
Non-surgical periodontal treatment
Antibiotics: Because bacteria cause periodontitis antibiotics may be prescribed as pills or as an Antibiotic fiber. The fibers are used in conjunction with scaling and root planing. They are placed directly into the pockets and are removed within 7-10 days later. Antibacterial mouth rinses may also be recommended to help plaque control. Bite correction: An imbalanced bite may accelerate bone destruction. Your teeth may be adjusted for proper and better function. A Bite-guard (removable retainer fitting over teeth) may be required to protect teeth surfaces and relax tense muscles. Splinting: This technique attaches weak teeth together, combining them into a stronger single unit, making them more stable and offering more comfortable chewing.
Surgical treatment
Flap Surgery: The periodontist separates the gum from the teeth creating a “flap” and accesses the infected pocket. It aims to reduce pocket depth and increase the ability to maintain the remnant pockets clean. In flap surgery, under local anesthesia, small incisions are made in the gum, so that it can be lifted back to expose the tooth and bone. The entire area is carefully cleaned. All tarter and infected granulation tissue are removed and the bone is examined. Because periodontal disease causes bone loss, often the bone will need to be recontoured in order for the gum to heal properly. When the procedure is done, the gums are sutured in to place on top the bone. The entire procedure typically requires from 1 to 3 hours to perform with only two quadrants of the mouth being address in a single visit. The sutures will remain in place for approximately one week, and you will likely be given a prescription for pain medication and antibiotics. Gingivectomy. This procedure is performed when excess amounts of gum growth around the teeth have occurred. This results in false pocket formation and the inability to keep them clean. Osseous (bone) surgery. This procedure is done to smooth shallow craters and defects in the bone due to mild or moderate bone loss. Guided Tissue Regeneration:This procedure is done in combination with a surgical flap operation where gum growth into a defect is barriered off to allow slower growing bone, cementum and ligament cells to populate a bony defect. Bone Grafts. Tiny fragments of the patient’s bone and synthetic bone are used to fill a bony defect around the teeth. These grafts act as a scaffold on or around which patients own bone is conducted or induced to grow.
Soft Tissue Graft. In cases of gum recession a graft is usually taken from the palate and transplanted onto the receding area to reinforce the thin gum and to inhibit further gum recession.
|
|